 Alaskans suffer from some of the most expensive health care costs in the nation. Medicare enrollees comprise about 14 percent of Alaska’s population and increases in Medicare spending from 2008 to 2018 have outpaced the national average. Despite having lower enrollment than other states, the federal government is spending substantially more for Alaskan’s Medicare benefits. How much more – and why?
Alaskans suffer from some of the most expensive health care costs in the nation. Medicare enrollees comprise about 14 percent of Alaska’s population and increases in Medicare spending from 2008 to 2018 have outpaced the national average. Despite having lower enrollment than other states, the federal government is spending substantially more for Alaskan’s Medicare benefits. How much more – and why?
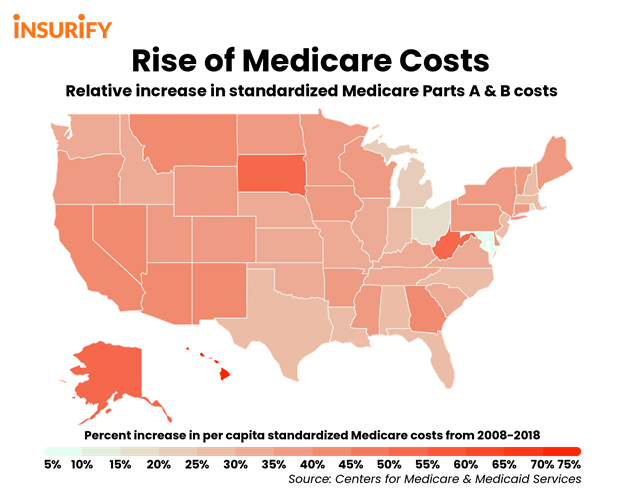
Insurify Insights recently released a ranking of the top ten states with the largest increases in Medicare costs from 2008 to 2018. The ranking includes spending on Medicare Part A, which covers inpatient care; and Medicare Part B, which encompasses outpatient services like medical tests, preventative checkups, annual wellness, and ambulance services. However, the ranking does not include the spending of Medicare Part D, which includes prescription drug coverage and is often a substantial cost to the federal government as well as states, as they are required to make contributions for Medicare Part D.
Alaska ranks third for increases in Medicare spending over 2008 to 2018. Alaska’s percent increase in per-capita Medicare costs was 53 percent. The report states that Alaska’s rate of growth in Medicare spending was 34 percent above the average growth rate for the United States, which may prove unsustainable in the long run. Alaska’s increase in beneficiary enrollment was only 14 percent, and Alaska’s change in per-capita standardized medical test costs was only 20 percent, both lower than the national average rate of growth.
Alaska’s increase in hospital readmissions was almost five percent. The growth rate in hospital readmissions was 48 percent above the nationwide average between 2008 and 2018. Hospital readmissions, which are usually measured as the number of patients previously seen for treatment that are readmitted to the hospital within 30 days, contribute to excess health care expenditures (in 2005, readmissions caused $15 billion in preventable Medicare spending nationwide), put patients at greater risk for hospital-acquired infections and medical errors, and reduce patient satisfaction.
The rising cost of health care and an increase in beneficiaries has led to often-staggering growth in Medicare spending. Nationwide from 2008 to 2018, standardized per-capita spending increased 35 percent. Enrollment in Medicare Part A and B rose by nearly 21 percent, while the standardized costs of medical tests per capita increased by a rate of nearly 27 percent. The report also found a significant correlation between hospital readmission rates and Medicare costs per-capita; in other words, when hospital readmissions increased, so did health care costs, though this connection may not necessarily be causal. In addition, beneficiary growth contributes to spending growth, but is not a statistically significant factor. In fact, the rates of increased enrollment and spending are significant, suggesting that growth in enrollment is more important than raw enrollment numbers in determining spending.
The ranking period from 2008 to 2018 does not include any increase in Medicare spending due to the COVID-19 pandemic, either, which could be considerable if more beneficiaries are enrolled, the cost of health care significantly increases due to the pandemic, or fraud consumes more of Medicare’s capacity. Notably, the federal government has loosened many Medicare regulations and waived policy controls designed to combat rampant fraud, though even cautious estimates place costs of Medicare fraud as around $52 billion in fiscal year 2017. However, Medicare has also began providing reimbursements for telemedicine and treatments in other non-traditional settings.
Controlling Medicare spending doesn’t mean skimping on care: it can be done while both improving patient outcomes and rewarding quality and efficiency. Reducing Alaska’s rate of hospital readmissions would stand to save patients from unpleasant and often-preventable treatments as well as save on Medicare costs. Further, moderating Medicare provider compensation toward national averages, particularly for specialty procedures, could help reduce Medicare spending; a 2017 Premera Blue Cross Blue Shield of Alaska study found that “payments to doctors and hospitals in Alaska are 76 percent higher than nationwide averages.”
Controlling Alaska’s rate of growth in Medicare spending is necessary: for patients, Alaska’s budget, and the federal budget. Insurify’s report defines the magnitude of the problems, and the particular areas, in which Alaskans should look for improvements.